Why Dr. Richardson Left Medicare
Why leave Medicare?
Why leave Medicare? This is probably one of the most common questions I get from my patients. And in the next few pages, I will attempt to answer this question from an objective standpoint. I know that may not be easy for you to understand. For, the system I left is the very same system which you are continuously led to believe benefits you.
Medicare PaperworkFor the seven years prior to my opting out of Medicare, the time I had been able to spend and the resources I had been able to devote to a high quality experience had been eroded by ever increasing administrative demands from both government and private insurance companies. Time I could previously spend face-to-face with my patients had to be spent on one of the myriad administrative “bean-counting” requirements of playing the insurance game.
All of this extra administrative demand did nothing to improve my patients’ experience or advance the care of their eyes. In fact, it resulted in the opposite: long wait times, more paperwork hassle, less face-to-face time in the exam room, and harried staff.
Inefficient Healthcare System
What follows below is by no means an exhaustive list. But I just want to give you a feel of how inefficient the current healthcare system can be, and how it ultimately penalizes you, the patient.
Non-value Added Administrative Work
Most Opthalmologists (57%) spend 5-14 hours on paperwork and other administrative tasks in a given week. About 10% of ophthalmologists spend at least 20 hours per week on non-patient-related activities.
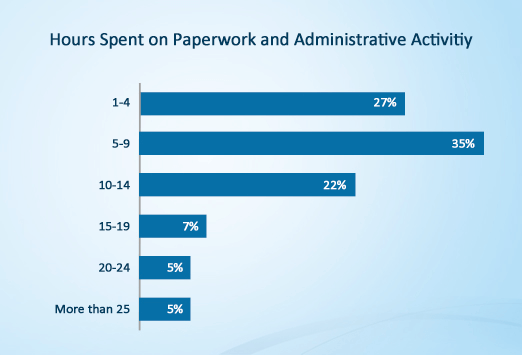
Source: Medscape Ophthalmologist Compensation Report: 2012
In my own practice, prior to leaving Medicare, my staff and I wasted roughly 3-4 hours/day doing non-value added administrative work.
Astronomical Paperwork
Each Insurance plan has its own contractual terms, prior authorization requirements, billing and claims rules, etc. On average, an ophthalmologist could easily have to deal with eight (8) insurance vendors. Can you just imagine the paperwork and documentation requirements!?
This paperwork problem, by the way, is not specific to ophthalmology. It spans all medical fields. The below quotation illustrates very well how complex a simple task can be under Medicare or Commercial Insurance.
The biggest problem with Medicare, anytime someone needs anything, the paperwork to get it done can be astronomical. Let’s say you have a patient who needs a nebulizer for their cardio-pulmonary obstructive disorder. They run between $60 and $120. To get that, you have to fill out this big form with all these questions, most of which have nothing to do with a nebulizer. So you have to pick out which questions are pertinent. Then you have to send it to a durable medical equipment supplier who then gets the patient a machine. It can be a seven to ten day turn around. Well, if the person is struggling with acute asthma or COPD, he doesn’t have seven to ten days. So we purchased six nebulizers and we keep them in the office. That way if someone needs a nebulizer long term, they borrow one of ours until they get one of their own.” [Dr. Slatosky]
But even paperwork required for more routine work adds to his costs. Dr. Slatosky estimates that for every 10 to 15 minutes he spends with a patient, he’ll spend a quarter to one-third of that on documentation and coding. He also has an employee who ensures that he has done the coding correctly in order to get paid. And it adds up, since he will have to do that for every patient he sees who has Medicare or private insurance.
Convoluted and Unnecessarily Complex Reimbursement System
The following list of acronyms and billing terms cover just a fraction of all the definitions, regulations, rules, government entities, and laws that a doctor must deal with in order to participate with Government and Commercial Insurances.
Acronyms and Billing terms
- ACA (Affordable Care Act, aka “Obamacare”)
- ACO (Accountable Care Organizations)
- “Allowable” Payment
- Attestation (for EHR Meaningful Use)
- “Bundling” of Physician and Hospital Payments (scheduled for 2013 in the ACA)
- Bundled Codes
- CERT (Comprehensive Error Rate Testing)
- CCI (Correct Coding Initiative)
- CMS (Centers for Medicare & Medicaid Services)
- Compliance plans (for Medicare)
- Conversion Factors
- CPT (Current Procedural Terminology)
- Downcoding
- EDI (Electronic Data Interchange)
- EHR (Electronic Health Record mandates)
- eRx Penalties
- Experimental (as a reason for service/testing denial)
- GPCI (Geographic Practice Cost Index – Medicare)
- Global Periods
- HCFA Forms
- HCPCS (Healthcare Common Procedural Coding System)
- Health Insurance Exchanges (as mandated by the ACA)
- HIPAA 5010
- ICD-9-CM (International Classification of Diseases 9th Edition Clinical Modification)
- ICD-10 (International Classification of Diseases 10th Edition)
- Incentives (Medicare)
- Interpreter Services
- IPAB (Independent Payment Advisory Board – as established by the ACA)
- Meaningful Use (with regard to EHR)
- Medical Necessity (as a reason for service/testing denial)
- Medicare Advantage Plans
- Medicare Rates
- MedPAC (Medicare Payment Advisory Commission)
- Modifiers
- MSPRCs (Medicare Secondary Payer Recovery Contractors)
- NCCI Edits
- Non-Covered Benefits
- OIG (Office of Inspector General)
- Penalties (Medicare)
- PQRS (Physician Quality Reporting System)
- RACs (Recovery Audit Commissions)
- RBRVUs (Resource Based Relative Value Units)
- RUC (Relative Value Scale Update Committee)
- Self audits
- SGR (Sustainable Growth Rate)
- “Take Backs” (by Medicare or Commercial Insurance)
- “Value-based” Physician Payment (as scheduled for 2015 in the ACA)
- ZPICs (Zone Program Integrity Contracts)
Does this give you a sense of just how convoluted and unnecessarily complex our current system of reimbursement is in the United States? I mean, really?!?
Cost estimates of inefficient health care claims processing, payment and reconciliation are between $21 and $210 billion. In the physician practice, the claims management revenue cycle consumes an unsustainable 10-14 percent of practice revenue.” – American Medical Association. June 2011. Standardization of prior authorization process for medical services.
Mind-boggling Coding System
Did you know that there’s a code for practically every conceivable medical scenario? If this weren’t a serious requirement for billing insurances, it would be ridiculously funny. “There is even a code for getting bitten by a dolphin, W5601XA. And for the swimmer that didn’t take the hint the first time, there is code W5601XD for getting bitten by a dolphin in a subsequent encounter.” Don’t believe me? Who could blame you.
Now, do you want your doctor spending time caring for you? Or, do you want your doctor spending time looking up the codes needed to bill for caring for you? Just as you don’t have unlimited time, neither does your doctor.
If your doctors are spending an enormous amount of time wading through the inefficient healthcare system, clearly, no one is spending sufficient quality time with you the patient.
And it doesn’t end here ….
Can you imagine any other business wherein 20%-30% of the time is spent on non-value added administrative work, tracking and reimbursing payments owed them? Probably not…
You deserve personalized care, more time, attention and compassion.
saturday Appointments Available. no outside referral needed.
