MicroPulse P3™ (MP3)
Cyclophotocoagulation
Non-incisional, Non-invasive Glaucoma Laser Treatment
Using Innovative Micropulse Technology!
What is MicroPulse P3™ (MP3)
“Cyclophotocoagulation”?
MicroPulse P3™ (MP3) “Cyclophotocoagulation” is a new type of minimally invasive glaucoma surgery (MIGS) that has quietly joined the fray in the battle against glaucoma. The procedure uses the Cyclo G6™ Glaucoma Laser System with MicroPulse P3™ Glaucoma Probe Device developed by Iridex. This innovative device was approved by the FDA only in 2015. It is the first safe, non-incisional, non-invasive laser for the treatment of glaucoma.
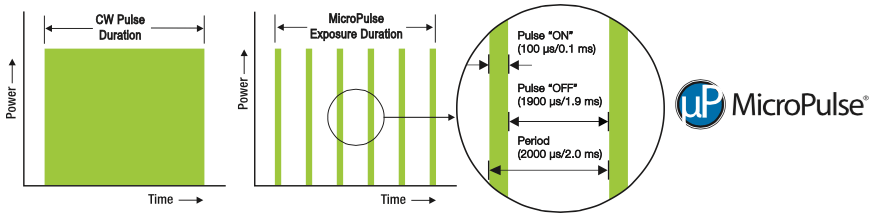
Traditional cyclophotocoagulation involves ciliary body destruction by using continuous wave laser to decrease the production of aqueous fluid and eventually intraocular pressure. MicroPulse P3™ Cyclophotocoagulation, however, delivers repetitive, low-energy diode laser “chopped” into ‘micropulses’ (or bursts) on the fluid-producing ciliary body. Each pulse heats up but does not burn or destroy eye tissue. In between each pulse is a pause. This pause allows the eye tissue to cool off. In this manner, the ciliary body is changed but not destroyed.
How Does MicroPulse P3™ (MP3) “Cyclophotocoagulation” Work?
It used to be a mystery how MicroPulse P3™ exactly works if it’s not actually destroying the ciliary body tissue. Dr. Murray Johnstone’s potentially solved this mystery recently. His poster presentation at the ARVO meeting in 2017 shows that MicroPulse P3™ actually shrinks the ciliary muscle (Note that the ciliary muscle does not produce intraocular fluid). This shrunken tissue pulls on the trabecular meshwork and Schlemm’s canal. This effectively stretches open the eye’s “drainage system” resulting to an improved aqueous outflow and thereby reduced Intraocular pressure.
So it seems that MicroPulse P3™ does not work via the same mechanism as Continuous Wave Cyclophotocoagulation. Rather, MP3 appears to work very much like the eye drop Pilocarpine. Pilocarpine is known to be an effective IOP lowering medication. However, Pilocarpine is seldom prescribed for open angle glaucoma as it must be dosed four times each day, is associated with brow ache, retinal detachment, and decreased night vision. MicroPulse P3™, on the other hand, requires only one or two treatments for sustained IOP reduction and is not associated with the side effects that are commonly experienced with Pilocarpine.
[Source: Johnstone M, Clinically used MicroPulse parameters induce outflow system configuration changes generally associated with improved aqueous flow. ARVO Annual Meeting Poster Presentation; 2017]
How Is MicroPulse P3™ Glaucoma Surgery Performed?
MicroPulse® P3 “Cyclophotocoagulation” can be performed in either an office or surgery center. The procedure can be done while in the supine (lying on back) position.
Once adequate anesthesia has been obtained and one is comfortably lying on his or her back, the eyelids are moved out of the way with either a lid speculum or the surgeon’s gloved fingers.
The MP3 laser probe is then gently guided along two semi-circular patterns around the front of the eye just beyond where the cornea meets the sclera (white part of the eye). The probe is passed back and forth multiple times.
The entire surgery takes only a few minutes.
- Non-Incisional & Non-invasive
- No bleeding and No infection risks
- Minimal to no inflammation post-op
- Patient downtime is significantly low
- Repeatable & Predictable
- Cost effective
How Well Does MicroPulse® “Cyclophotocoagulation” Work?
Micropulse (Iridex), is a new transscleral diode laser CPC platform that appears to have a better safety profile than traditional Cyclophotocoagulation. It has appeared on 7 peer-reviewed publications, 60+ studies, clinical posters and presentations and has short and long term (78 months) compelling clinical evidence, in which IOP reduction was reported in the range of 20-50%. At the recent American Glaucoma Society (AGS) 2017 Annual Meeting, 10 posters reported success rate from 50% – 80% and the incidence of reported side effects was low, with cystoid macular edema and loss of ≥2 lines of BCVA the most common. Below are some of the studies:
- Tulane Study Grp - @ 5 mos.
- Shazly et al - @ 6 mos.
- Radhakrishan et al - @ 6 mos.
- Emanuel ME et al - @ 12 mos,
- The Yale Study - @12 mos
- NUH Study @18 mos.
- NUH Study @ 78 mos.
- Additional Studies
Dr. Yelenskiy and colleagues (Tulane Study Group) looked at early results of using MP3 on 163 patients with “intractable glaucoma”. In other words, the glaucoma was not responding to treatment. Traditionally these patients would be advised to have either trabeculectomy (“trab”) or glaucoma drainage device (“tube”).
Surgical Success, defined as a IOP greater than 6mmHg but less than 18mmHg or 20% reduction was 83%. The average IOP dropped from 21.5mmHg to 16.5mmHg. The average number of glaucoma medications dropped by 50%. Average vision was not significantly different after surgery.
Only 10% of patients required a second treatment of Micropulse® Laser Trans-Scleral Cyclophotocoagulation. However, 15% of patients did eventually require additional glaucoma surgery.
Risks and complications included:
- post-operative pain (56%),
- inflammation (36%), and
- macular edema/swelling (<2%)
These results are impressive, even more so given that almost all (if not all) of these patients would have otherwise gone on to riskier surgeries such as trabeculectomy, glaucoma drainage device, or continuous wave cyclophotocoagulation. The study, however, does suffer from the following weaknesses: retrospective chart review design and short duration of follow-up (an average of just over 5 months).
Source: Micropulse Laser Trans-Scleral Cyclophotocoagulation – The Tulane Study Group Results
Thirty two patients (34 eyes) with multiple types of (medically uncontrolled) glaucoma ranging from primary open angle glaucoma (POAG) to neovascular glaucoma (NVG) were enrolled in the study conducted by Dr. Tarek A. Shazly and colleagues. Success was defined as a drop in intraocular pressure (IOP) of at least 20%. Six months after surgery the 82% of eyes met the criteria for success. The average IOP dropped from 29.2mmHg to 13.3mmHg. The need for glaucoma medications was also reduced (on average) from 3.3 to 2.4.
Five patients (15%) required a second treatment of Micropulse Transscleral Cyclophotocoagulation after a mean duration of 64.8 days after the initial treatment. Six patients (18%) required additional surgery. There were no reported complications.
Sources: New-Glaucoma-Treatments.com • Shazly T, Loewen N, Polast J, Conner I. Outcomes of Micropulse Transscleral Cyclophotocoagulation in Medically Uncontrolled Glaucoma. American Glaucoma Society 27th Meeting Poster Presentation; 2017
One hundred forty four patients (166 eyes) with a wide variety of glaucoma types were included in the study. However, the length of this study was short with six month data available for less than one half of study participants.
Average IOP decreased from 22mmHg to 16.7mmHg with a mild decrease in number of medications needed from 3.6 to 3.0. Fifty eight percent (58%) of eyes were considered to have met the definition of “success” (essentially a 20% reduction in IOP). The 42% who failed treatment were evenly divided into those who required additional surgery and those who simply did not achieve a 20% reduction in IOP.
Success appeared to be more likely among female patients and those who received longer duration treatment. Higher initial IOP and severity of glaucoma seemed to be associated with greater risk of failure.
The most common complications included:
- pupil dilation (11%),
- corneal surface drying (7%),
- significant inflammation (3%),
- swelling of the macula (2%), and
- decreased near vision (2%).
One patient in the study (0.6%) did experience a permanent reduction in vision. Of interest is that this patient had received the lower duration treatment.
In summary, this study supports the potential value of Micropulse Cyclophotocoagulation (MP3) at earlier stages of glaucoma. It also reveals that this “gentler” surgery is not without a small risk of vision loss.
Sources: New-Glaucoma-Treatments.com • Abstract: Radhakrishnan, Sunita, Wan J, Tran, B, Thai, A; Outcomes Of Micropulse Cyclophotocoagulation – A Multicenter Review. American Glaucoma Society 27th Meeting Poster Presentation; 2017 Source: http://new-glaucoma-treatments.com/micropulse-cyclophotocoagulation-mp3-glaucoma-treatment-at-earlier-stages-of-glaucoma/
A retrospective chart review was performed for all patients who underwent a MP-TSCPC at the Glaucoma Associates of Texas. A total of 84 eyes were treated with MP-TSCPC in this study.
- Mean intraocular pressure (IOP) dropped from 27.7 mmHg to 11.1 mm Hg @ 12 months follow up
- Mean number of medications dropped from 3.3 to 2.3 @ 12 months follow up
- Five patients required further laser or surgical intervention for adequate IOP control.
- Complications included hypotony, IOP spike, hyphema, serous choroidal detachment, persistent inflammation (at 3 months, inflammation was still present in 46% of eyes), and vision loss (vision loss of at least 1 line was present in 41% of eyes)
MP-TSCPC is effective at lowering IOP and decreasing the need for ocular antihypertensive medications. Eyes with limited visual potential or at high risk for incisional glaucoma surgery can successfully be treated with MP-TSCPC as a reasonable and effective alternative to traditional CPC.
Source: Emanuel ME, Grover DS, Fellman RL, Godfrey DG, Smith O, Butler MR, Kornmann HL, Feuer WJ, Goyal S. Micropulse Cyclophotocoagulation: Initial Results in Refractory Glaucoma. J Glaucoma. 2017 Aug;26(8):726-729. doi: 10.1097/IJG.0000000000000715. PubMed PMID: 28671927.
Doctors Alexander Nguyen and Robert Noecker reviewed the charts of 95 patients with glaucoma who had undergone Micropulse Trans-scleral Cyclophotocoagulation and had been followed for at least a year after surgery.
The average IOP prior to this glaucoma treatment was 25.1mmHg. One year after MP3 the average IOP dropped to 17.4mmHg (30.7% reduction). Additionally, the need for glaucoma medications decreased by 50%. Of particular interest is that, on average, MicroPulse P3™ reduced intraocular pressure (IOP) as well as need for IOP-lowering medications at every post-operative visit. In other words, the benefit was both immediate and long-term.
Retreatment was necessary in 23% of those who had MP3. The most common side effect was inflammation which was present early after surgery. No one in this study experienced long-term inflammation or hypotony (IOP that is too low). A sustained increase in pupil size was noted in 3 patients (0.3%).
In summary, Micropulse Trans-scleral Cyclophotocoagulation appears to be a relatively safe and effective treatment of glaucoma with both short and long-term benefit.
Source: One-Year Results of Micropulse Trans-scleral Cyclophotocoagulation – Yale Study
NUHS Study – 45% IOP reduction at 18 months
Dr. Maria Cecilia Aquino & Prof Paul Chew of National University Health System, Singapore conducted this study to compare the efficacy and safety of micropulse and continuous wave diode transscleral cyclophotocoagulation in refractory glaucoma.
Twenty three (23) patients underwent micropulse diode transscleral cyclophotocoagulation (MPCPC). Surgical Success, defined as between 6 and 21 mmHg and at least a 30% reduction was 75% at 12 months and 52% at 18 months (29% and 30% respectively for CWDTC treated eyes). The mean intraocular pressure was reduced by 45% after 17.5 ± 1.6 months (range 16–19) follow up. No significant difference in retreatment rates or number of intraocular pressure lowering medications was noted between MPCPC and CWDTC. However, the ocular complication rate was higher in continuous wave diode transscleral cyclophotocoagulation treated eye.
CONCLUSION:
Diode transscleral cyclophotocoagulation in both micropulse and continuous modes was effective in lowering intraocular pressure. The micropulse mode provided a more consistent and predictable effect in lowering intraocular pressure with minimal ocular complications.
NUHS Follow-up Study – 39% IOP reduction at 78 months
Dr. Maria Cecilia Aquino & Prof. Paul Chew of National University Health System, Singapore conducted this study to evaluate and present the long-term efficacy of micropulse diode transscleral cyclophotocoagulation (MPCPC) in subjects with refractory glaucoma treated from a prior prospective study.
There were 14 patients (61%) out of the 23 treated with MPCPC in the prior randomized study who had follow-up review up to 78 months. This retrospective review was limited by the small number of sample size and the attrition rate after many years of follow-up.
Significant IOP reduction was observed at all time points compared to pre-treatment IOP. No significant difference in eye drops noted pre & post laser. Micropulse diode transscleral cyclophotocoagulation was effective in the long term IOP control of refractory glaucoma.
MP3 Clinical Outcomes Summary at 78 Months | Mean IOP (n=14)
- 39% mean IOP reduction at 78 months
- Reduction in eye drops from mean of 1.8 to 1.1
- On average 3.6 treatments per patient with MP3 probe
Additional Studies Provide Consistent Outcomes
- Dr. Robert Noecker, n=46, 41% IOP reduction @ 12 months follow-up.
- Wills Eye Hospital, n=19, 30% IOP reduction, reduction in eye drops: 3.3 to 1.8 @ 6-12 months follow-up.
- Dr. Thomas John, n=20, 30% IOP reduction @ approximately 2 months follow-up.
- Doheny Eye Center UCLA, Dr. Brian Francis, n=20, 43% IOP reduction @ approximately 2 months follow-up.
- University of Missouri, Dr. Rohit Krishna, n=30, 43% IOP reduction @ 6 months follow-up.
- Wills Eye Hospital, Dr. Marlene Moster, n=78, 50% IOP reduction @ an average of 7.5 months follow-up.
- Toyos Clinic, Dr. Melissa M Toyos and Dr. Rolando Toyos, n=26, 30% IOP reduction, reduction in eye drops: 3.3 to 1.8 @ 6-12months follow-up. (All patients had previously undergone uncomplicated phacoemulsificDtion and SLT or MLT. Most (18/26) of the eyes were severe or end-stage glaucoma. )
- Minnesota Eye Consultants, Drs. Thomas Samuelson and Mark Hansen, Reviewed 119 procedures and concluded that “MicroPulse is an effective, non-invasivetreatment to lower IOP and is a viable option for all types of glaucoma atvarious stages.”
- University of Washington, Dr. Murray Johnstone “Clinically used MicroPulse parameters induce outflow system configuration changes generally associated with improved aqueous flow.”
- UCSF, Dr. Shan Lin “No presence of suprachoroidal fluidor anatomical changes were found.” The study concluded, “MP-TCP is effective at lowering IOP in the majority of patients and appears safe without major complications.”
- Nisha Chadha, MD; Cataract & Refractive Surgery Today; September 2017 – New Laser Therapies For Glaucoma- “…MicroPulse technology offers a novel meansof laser delivery that has been shown to be safe and effective…”
- Matthew E. Emanuel, MD Glaucoma Journal; Aug 2017 – MicroPulse Cyclophotocoagulation: Initial Results in Refractory Glaucoma- “…The out comes of our study arepromising with good evidence of the IOP-lowering effects of MP-TSCPC anddecreased need for ocular antihypertensive medications postlaser at 6 months…”
What are the side effects of MicroPulse P3™ Cyclophotocoagulation?
MicroPulse P3™ Cyclophotocoagulation uses less energy than Continuous Wave Cyclophotocoagulation. This reduction in energy translates into less damage to eye tissue, reduced inflammation, diminished post-op pain, and fewer risks. The procedure is also non-invasive, easily undertaken, and well tolerated with transscleral application, eliminating bleeding and postoperative infection risks. Often, postoperative inflammation and pain are insignificant and hospital admission is not required. Some of the small percentage of reported risks in previous studies include: pupil dilation, corneal surface drying, significant inflammation, swelling of the macula, and decreased near vision. Given the higher risk of both non-treatment or traditional glaucoma surgical treatment (trabs and tubes), MP3 still appears to be a welcome and overall lower risk addition to the available surgical glaucoma treatments.
Does MicroPulse P3™ Cyclophotocoagulation hurt?
No. During the surgery your eye will be anesthetized. Although there can be some discomfort during the laser application, the procedure is generally not painful.
However, unlike other glaucoma laser procedures (such as laser trabeculoplasty), MP3 requires more than just topical anesthetic drops in order to minimize discomfort. Either a local anesthetic “block” (injection around the eye) or intravenous (IV) sedation can be used to achieve adequate comfort during the procedure.
What happens after MP3 Cyclophotocoagulation surgery?
After surgery the eye may be a little sore. Generally this is mild enough that it can be relieved with acetaminophen or anti-inflammatory eye drops. The eye may also be red after MP3 glaucoma surgery. This is because delicate blood vessels on the surface of the eye may bleed just from the movement of the laser probe along the surface of the eye (especially in those who are taking blood thinners). This is only of cosmetic concern and will resolve on its own within a week or two of surgery.
If IV anesthesia was used then one can expect to be a bit groggy the afternoon of surgery (plan on napping). By the next day, however, most everyone who has chosen MP3 is without significant discomfort or pain.
Unlike many glaucoma surgeries, there are no restrictions on one’s activities after MicroPulse P3™ Cyclophotocoagulation. Nonetheless, it may be prudent to avoid heavy lifting for at least a few days after surgery.
Your surgeon will likely want to see you in his or her office within the first week after surgery. Your IOP may or may not be lower at this first post-operative visit. By one to three months after MP3, however, IOP lowering should be observed. If the IOP is still elevated then a second treatment may be necessary to achieve a reduction in IOP.
Who Is a Candidate For MicroPulse P3™ Laser Treatment?
The combination of IOP lowering benefit, low risk profile, and likely reimbursement by commercial insurances and Medicare makes MicroPulse® P3 “Cyclophotocoagulation” a good option for almost all patients with glaucoma who fit into any of the following categories:
- Those with poorly controlled IOP despite using all available glaucoma medications
- Those who have difficulty tolerating glaucoma medications
- Those who have difficulty affording their glaucoma medications
- Those who have difficulty regularly taking their glaucoma medications
- Those who have already had Laser Trabeculolplasty
- Those who are physically unable to tolerate more extensive glaucoma surgery
What Top Glaucoma Surgeons Are Saying
The MicroPulse P3 device has given me over 30% IOP lowering. With patients that are non-compliant with their medication, or we are really trying to keep off their medication, the MicroPulse P3 device allows me to treat patients more aggressively.
I have found the MicroPulse P3 to be a non-incisional, easy, andsafe way to reduce pressure anytime my patients need it, and it ispredictable and highly efficacious.
The MicroPulse P3 device has benefits for both the surgeon and the patient: it can be used in the office or the operating room, and there is no major recovery time for the patient. The MicroPulse P3 device can serve a variety of patients. In some patients who cannot take medications, IOP can be controlled and medications replaced. In other patients, IOP can be controlled; allowing the patient to maintain his or her quality of life (or life plans) without having to undergo incisional surgery. For patients at high risk of complications from incisional surgery, this device can provide a safe alternative. I have been impressed that it works well in exfoliation and angle-closure eyes. Finally, I have found that the MicroPulse P3 device complements prior tube shunt procedures, possibly by providing a dual-mechanism synergy to the aqueous outflow afforded by the tube.
Micropulse Trans-scleral Cyclophotocoagulation appears to be a relatively safe and effective treatment of glaucoma with both short and long-term benefit. Given the higher risk of both non-treatment or traditional glaucoma surgical treatment (trabs and tubes), MP3 still appears to be a welcome and overall lower risk addition to the available surgical glaucoma treatments.
I have been impressed that the MicroPulse P3 therapy with the CycloG6 can deliver pressure lowering in a broad range of glaucomas,including mild and moderate patients who I want to free from theadverse effects of drops.
The MicroPulse P3 device has become an essential part of my armamentarium for use in glaucoma surgical procedures. It provides a very safe and efficacious solution for IOP control. I have used MicroPulse P3 for some of my most complicated cases but also I feel comfortable enough using it for patients with earlier disease in which we want to avoid a filtering bleb or the placement of hardware in the eye.
LATEST ARTICLES ON DR. RICHARDSON’S GLAUCOMA HEALTHHUB
See If MicroPulse P3™ (MP3)
Cyclophotocoagulation Is for You
David D. Richardson, MD, is a board-certified Ophthalmologist specializing in the treatment of cataract and glaucoma. He is also recognized as one of the most highly skilled cataract and glaucoma surgeons in the US and is among an elite group of glaucoma surgeons in the country performing the highly specialized, minimally-invasive glaucoma surgery (MIGS), canaloplasty. Morever, Dr. Richardson is one of only a few surgeons in the greater Los Angeles area that performs MicroPulse P3™ Cyclophotocoagulation (MP3) glaucoma laser surgery.
Call today to schedule an appointment with Dr. Richardson at
(626) 289 7856