Get Your Corneal Hysteresis Number Using The Ocular Response Analyzer G3
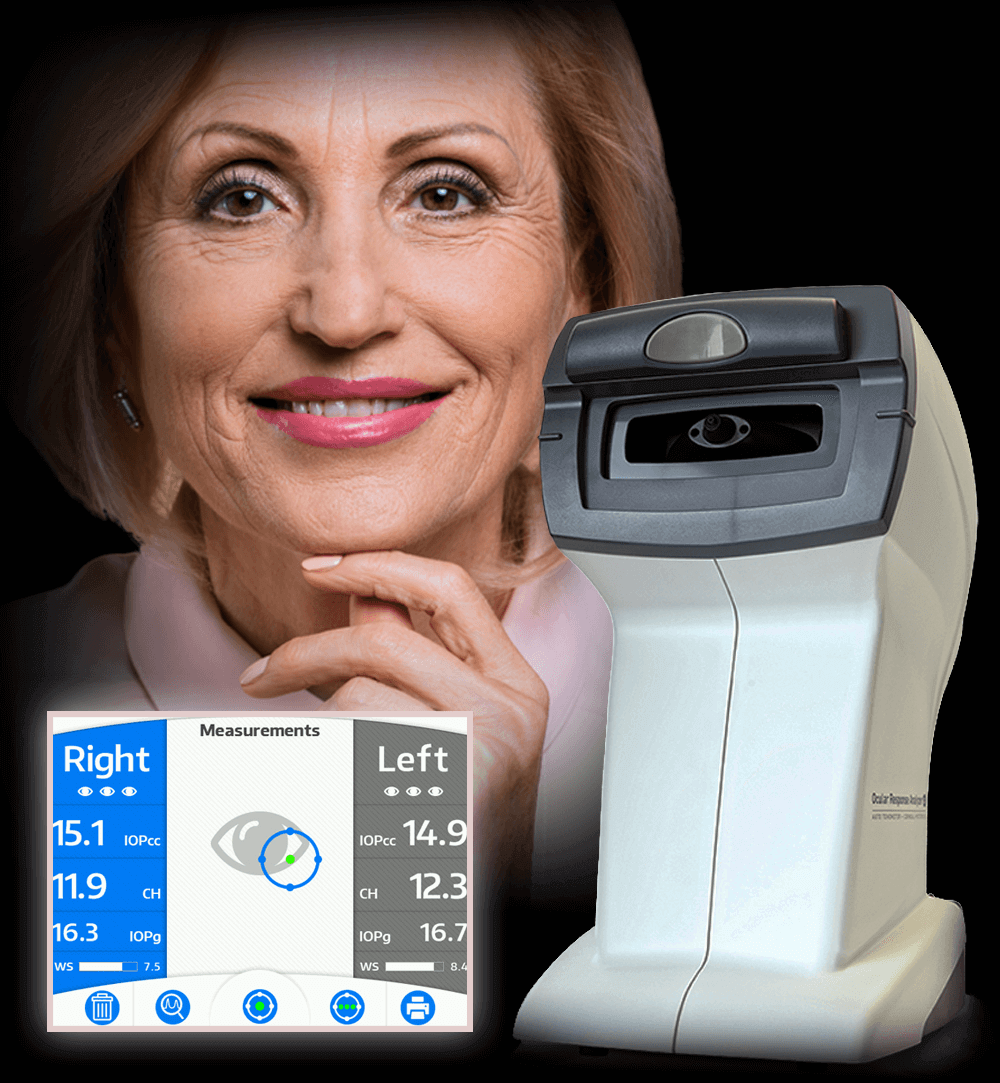
Dr. David Richardson has recently acquired the Reichert Ocular Response Analyzer (ORA).
The Ocular Response Analyzer (ORA) is the only instrument in the world capable of measuring Corneal Hysteresis (CH), a superior predictor of glaucoma progression

Measure Beyond Intraocular Pressure (IOP) and Central Corneal Thickness (CCT)
No corneal parameter has been shown to be more important in glaucoma decision making than
CORNEAL HYSTERESIS
What is Corneal Hysteresis?
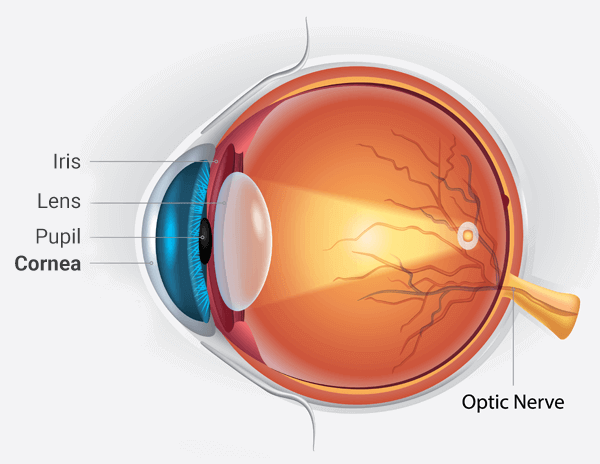
The cornea is the clear (transparent) surface at the front of the eye which focuses light onto the lens inside the eye. It can be thought of as a half-millimeter thick soft contact lens. Like a soft contact lens, it is deformable (“bendy”). Many biological tissues that can be flexed or bent without permanent damage can be described as “viscoelastic”. Viscoelastic tissues absorb some of the force used to deform them like the suspension strut in your car or truck works to absorb the impact of a pothole.
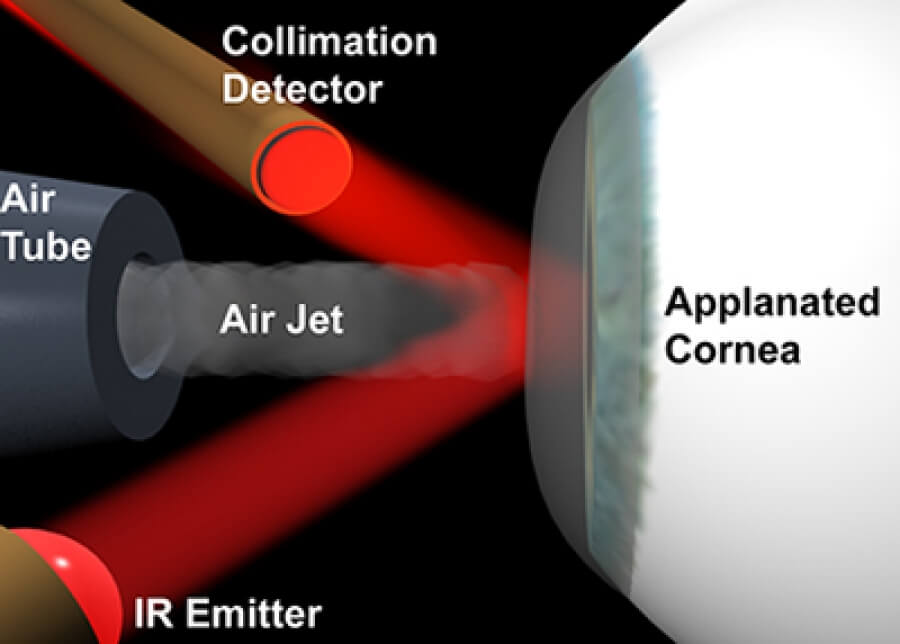
Corneal hysteresis essentially measures the “shock-absorbing” ability of the cornea. The higher the corneal hysteresis, the greater the shock-absorbing capacity of the cornea (and perhaps the eye). This is very different from thickness or topography, which are geometrical attributes of the cornea.
Corneal Hysteresis and Glaucoma
Low central corneal thickness (CCT) measurements are known to be associated with glaucoma risk. However, corneal hysteresis is more strongly associated with glaucoma presence, risk of progression[1], and effectiveness of glaucoma treatments than central corneal thickness. Thus, if you could choose only one corneal measurement, you would be wise to choose Corneal Hysteresis over central corneal thickness.
A low corneal hysteresis:
- Can help predict who might develop glaucoma[2]
- Is more common in eyes with glaucoma than otherwise normal eyes
- Is associated with optic nerve and visual field damage[3] in those with glaucoma
- Increases the risk of further damage to the optic nerve[4]
- Increases the risk of progressive visual field loss[5]
- May help in predicting which patients with normal tension glaucoma are more likely to lose vision[6]
- May predict who will respond to certain IOP lowering therapies. For example, a low corneal hysteresis is associated with a greater reduction of IOP after treatment with a class of IOP lowering eye drops known as the prostaglandin analogs (latanoprost being the most common)[7]. This also appears to be the case with certain surgical treatments such as selective laser trabeculoplasty (SLT)[8].
References
[2] A Prospective Longitudinal Study to Investigate Corneal Hysteresis as a Risk Factor for Predicting Development of Glaucoma. AJOPHT 10365 – in press. Feilin Zhu , Alberto DinizFilho, Linda M. Zangwill , Felipe A. Medeiros
[3] Congdon NG, Broman AT, Bandeen-Roche K, Grover D, Quigley HA. Central corneal thickness and corneal hysteresis associated with glaucoma damage. Am J Ophthalmol. 2006 May;141(5):868-75.
[4] Zhang C, Tatham AJ, Abe RY, Diniz-Filho A, Zangwill LM, Weinreb RN, Medeiros FA. Corneal Hysteresis and Progressive Retinal Nerve Fiber Layer Loss in Glaucoma. Am J Ophthalmol. 2016 Jun;166:29-36
[5] Medeiros FA, Meira-Freitas D, Lisboa R, Kuang TM, Zangwill LM, Weinreb RN. Corneal hysteresis as a risk factor for glaucoma progression: a prospective longitudinal study. Ophthalmology. 2013 Aug;120(8):1533-40.
[6] Park JH, Jun RM, Choi KR. Significance of corneal biomechanical properties in patients with progressive normal-tension glaucoma. Br J Ophthalmol. 2015 Jun;99(6):746-51.
[7] Agarwal DR, Ehrlich JR, Shimmyo M, Radcliffe NM. The relationship between corneal hysteresis and the magnitude of intraocular pressure reduction with topical prostaglandin therapy. Br J Ophthalmol. 2012 Feb;96(2):254-7.
[8] Hirneiß C, Sekura K, Brandlhuber U, Kampik A, Kernt M. Corneal biomechanics predict the outcome of selective laser trabeculoplasty in medically uncontrolled glaucoma.Graefes Arch Clin Exp Ophthalmol. 2013 Oct;251(10):2383-8.
Ocular Response Analyzer® (ORA) is the only device cleared by the FDA that measures
Corneal Hysteresis (CH), a superior predictor of glaucoma progression
Corneal Hysteresis Measurement Using
Reichert Ocular Response Analyzer
at San Marino Eye
Modern Glaucoma Risk Assessment at San Marino Eye
Dr. David Richardson uses the FDA-approved Ocular Response Analyzer G3 (ORA) to measure the Corneal Compensated Intraocular Pressure (IOPcc), a better indication of the true pressure and Corneal Hysteresis (CH), a superior predictor of glaucoma progression.
- Non-contact. No topical anesthesia and/or fluorescein
drops needed. - Comfortable patient positioning. No chin rest.
- Patented softest possible air pulse, ensuring maximum patient comfort.
- Very Quick and accurate measurement.
- Proudly Made in the USA.
Reichert Ocular Response Analyzer
The Reichert Ocular Response Analyzer is easy and convenient for the the patient. Patient positioning is easy and comfortable thanks to the left – right sliding headrest, and the easy to find fixation target. Best of all, the ocular response analyzer utilizes a non-contact measurement methodology. So no anesthetic is required.
What Some of The Top Ophthalmologists Are Saying
Certainly, hysteresis tells me about a patient’s risk, just as a thinner or thicker cornea does. A patient whose hysteresis is lower than, say, 9 mmHg is at greater risk of progression. If a patient has a higher hysteresis, I worry less, even if his pressure is elevated.
Hysteresis is a very powerful risk factor for progression of the disease, and I think it’s one that’s largely overlooked. In fact, if you take Hysteresis out of the central corneal thickness measurement, central corneal thickness might not even be a risk factor for glaucoma progression. Hysteresis is absolutely critical for estimating the risk.
In a prospective, longitudinal study, my colleagues and I found that patients with lower hysteresis had significantly faster rates of progressive visual field loss compared to those with higher hysteresis. Importantly, the hysteresis measurements had a stronger ability to predict visual field progression than measurements of corneal thickness.
I have decided that the measurement of corneal hysteresis is important enough to provide to my patients with glaucoma or who might be at risk for glaucoma. This includes anyone with elevated IOP, suspicious appearing optic nerves, family history of glaucoma, history of diabetes, history of myopia (“nearsighted”). If you fall into one of these (or other glaucoma risks) categories and have not yet obtained a measurement of corneal hysteresis, I encourage you to make an appointment with a doctor in your area who has this important technology.
Want To Know More About Corneal Hysteresis?
LATEST ARTICLES ON DR. RICHARDSON’S GLAUCOMA HEALTHHUB
…But there are also vital signs of the eye. Visual acuity (e.g., “20/20”) and intraocular pressure (IOP) are two such measurements. For the last twenty years, those with ocular hypertension or glaucoma have had a third vital sign: central corneal thickness (CCT). Corneal thickness can be used (among other things) to estimate how likely someone may be to develop glaucoma. However, a newly discovered measurement has proven to be even more valuable than CCT. This new measurement is called Corneal Hysteresis (“CH”)… [Read more →]
Corneal Hysteresis Evidence in Glaucoma
Approximately 700 publications since 2005! Here are a few…
Taking Glaucoma Risk Assessment to the Next Level: The Role of Corneal Hysteresis
Read PDF version via doclibrary.com

Corneal hysteresis and its relevance to glaucoma
Read PDF Edition via journals.lww.com
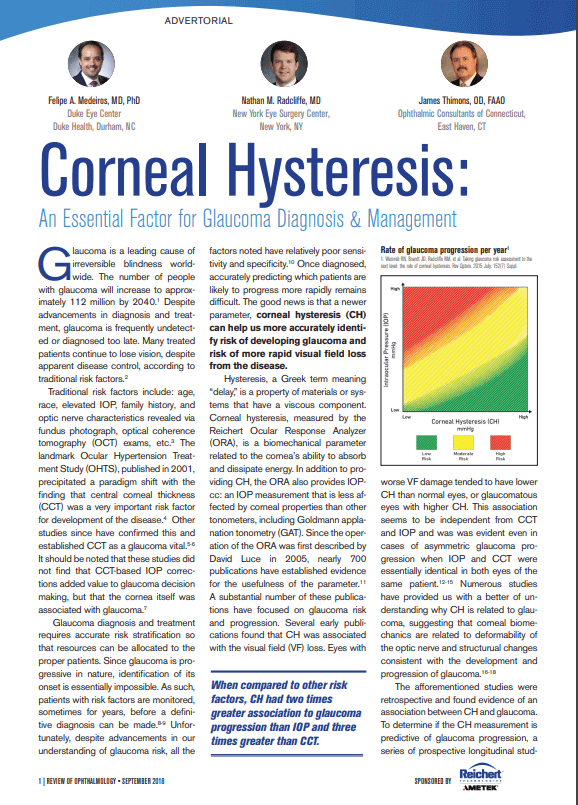
Corneal Hysteresis: An Essential Factor for Glaucoma Diagnosis and Management.
parameter, corneal hysteresis (CH) can help us more accurately identify risk of developing glaucoma and
risk of more rapid visual field loss from the disease.
Read PDF Edition via doclibrary.com
Corneal hysteresis and primary open angle glaucoma
Read PDF Edition via www.ncbi.nlm.nih.gov
A New Glaucoma "Vital Sign": How Corneal Hysteresis is Improving Glaucoma Patient Management.
More recent studies on CH have confirmed the importance of the cornea in glaucoma decision making and have shed light on the role of corneal biomechanics, as opposed to simply central corneal thickness (CCT).
Read PDF Edition via www.reviewofophthalmology.com
Make an Appointment
with Dr. Richardson
and Get “your CH number”
Dr. David Richardson provides IOPcc and Corneal Hysteresis
Measurements at his Marino Eye office.
Get a modern glaucoma risk assessment.
Make an appointment with Dr. David Richardson now.
Call today to schedule an appointment at
(626) 289 7856