Cataract Surgery Risks and Complications
Possible Cataract Surgery Complications and Why You Need to Know What IOL Your Eye Surgeon Will Implant During Cataract Surgery
Cataract Surgery Problems and Complications
The development of cataracts is inevitable for most anyone who lives long enough. The treatment of cataracts is to surgically remove and replace the hazy natural lens with a clear synthetic intraocular lens (IOL) implant. Fortunately, cataract surgery is one of the safest and most effective types of surgery. Serious problems or complications are rare. Indeed, cataract surgery has a very high success rate with approximately 97% of people experiencing no cataract removal complications. That being said, all surgeries have risks and surgeries on the eye come with the risk of loss of vision.
No doubt you have friends or family with cataracts who have already undergone cataract surgery. They may have told you that this only a minor surgical procedure and given you the false impression that it is a totally risk-free operation. It is important to emphasize that before having any surgery on your eyes you will need to come to grips with the fact that, although rare, occasionally patients experience complications that can limit vision after cataract surgery. Many of the risks associated with cataract surgery can occur by chance after what may have seemed like a successful eye surgery. With cataracts, the question you must ask is whether your vision is bothering you enough that you feel it is worth taking these real, but unlikely, risks of cataract surgery.
If your cataracts are affecting your daily activities, then coming to terms with these rare complications might be the only way to stop poor eyesight from interfering with your life. If your vision problems are so severe that they interfere with your daily life, your cataracts may need to be removed. Eye surgery (what is called “extracapsular cataract extraction”) is the only way to remove cataracts. To date, cataract removal cannot be done with eye drops or a laser procedure (though a special type of laser can be used to “assist” the surgeon). You may decide not to have the cataract removed. If you choose to delay the surgery it is unlikely that you would permanently harm the eye, but your vision loss from the cataract will continue to get worse as it would with any other chronic, progressive eye disease.

Problems Encountered During Cataract Surgery
Femto Laser Assisted Cataract Surgery (FLACS) Complications
There are essentially two main types of cataract surgery available in the United States: standard manual phacoemulsification and Femto Laser Assisted Cataract Surgery (FLACS). Although there are very few additional risks of FLACS compared to standard cataract surgery, it does require additional equipment which can, on occasion, fail to perform as desired. The most common risk of FLACS is that the procedure must be aborted. If so, it is usually still possible to remove the cataract using manual cataract surgery.
Complications of Anesthesia
Most patients cannot tolerate cataract procedures without first numbing the eye. Anesthesia is generally performed with eye drops, but occasionally an anesthetic injection must be administered next to or behind the eye. As you might imagine, placing a sharp needle next to the eye risks puncturing the eye which could then lead to complications such as bleeding in the eye, infection, retinal detachment, and loss of vision. Rarely, the anesthetic agent may be injected directly into a blood vessel leading to the brain. Although death from cataract surgery is exceedingly unlikely, this is one of the complications that can result in loss of life. For this reason anesthetic injection around the eye is falling out of favor among many surgeons.
Capsular Tear
The eye’s natural lens is held in position behind the iris in a bag-like structure called the capsular bag. The lens capsule is a delicate membrane and occasionally tears. A small tear in the capsule may not be associated with any additional risks or eye problems. Larger tears, however, can limit your surgeon’s ability to properly position the intraocular lens (IOL) in the bag which may require placing a lens in front of the iris into the “anterior chamber” of the eye. A posterior capsule tear may also be associated with increased post-operative risks such as infection, swelling of the retina (“cystoid macular edema”), or retinal detachment.
“Dropped” Lens
To remove the cataract, the natural lens must be broken up into small fragments that are then removed from the eye through a very small tube. If the capsule is torn then pieces of the cataract (“lens fragments”) may slip into the back portion of the eye.
Aborted Implantation of an Intraocular Lens
The lens in the eye serves the important role of focusing light onto the retina. If a cataract is simply removed without being replaced by a lens implant, the vision will continue to be blurred after surgery until the residual refractive error is corrected. Sometimes, however, the surgeon cannot safely place an artificial lens into the eye at the time of cataract surgery. This may be due to an intraoperative complication (such as a torn posterior capsule) or it may just be that the patient’s anatomy did not support placement of the IOL. If a lens cannot be placed at the time of initial cataract surgery then a separate procedure will be necessary to position or even sew in an IOL.
Intraoperative Floppy Iris Syndrome “IFIS”
Prostate disease in men and urinary problems in women are often treated with a class of medication known as the alpha-blockers. Flomax® (or tamsulosin) is the most commonly prescribed of this class. Even one dose of tamsulosin can result in a condition called Intraoperative Floppy Iris Syndrome “IFIS”. Your doctor may ask about any history of using this drug class as it is one of the more common risk factors for developing a complication during cataract surgery. During IFIS the pupil constricts and becomes “floppy”. This reduces the surgeon’s view of the cataract, and is known to increase the intraoperative complications of cataract surgery such as posterior capsule rupture. Fortunately, there are medications and techniques that your eye doctor can use during surgery to reduce the risk of IFIS.
Problems Encountered After Cataract Surgery
Pain
Cataract surgery is usually quite comfortable. Following cataract surgery mild discomfort is typical, but severe pain is extremely unusual. You should inform your surgeon about any eye pain or headache that does not resolve with acetaminophen or the drops prescribed by your eye doctor.
Increased Pressure in the Eye
Intraocular pressure (IOP) spikes are fairly typical following any intraocular surgery. One common cause of increased eye pressure after cataract surgery is temporarily retained viscoelastic. Your eye doctor uses this jelly-like substance to facilitate placement and positioning of the artificial lens. The thick consistency of viscoelastic can reduce outflow of the eye’s aqueous fluid, causing a pressure spike that generally peaks about six hours after surgery, then subsides. Intraocular inflammation after cataract surgery may also increase risks of pressure spikes. Your ophthalmologist may prescribe topical medications to lower the IOP.
Wound leaks
Cataract surgeries are performed through very small incisions in the cornea. These incisions usually “self-seal”, but not always. A leaky incision is a risk factor for development of an eye infection. There are a number of treatments for a wound leak including prescription medications, placement of a “bandage contact lens”, or placing a suture in the cornea (a minor surgical procedure).
Corneal Edema or Inflammation (swelling)
The energy used to break the cataract into smaller lens fragments is absorbed by the cornea. This may result in inflammation or swelling that generally goes away after a few weeks. Patients who have an unhealthy cornea prior to surgery or have a very dense cataract may experience increased swelling and may need additional medical or surgical treatment. Occasionally a corneal transplant is required to address persistant corneal swelling.
Inflammation Inside of the Eye
There will be some inflammation after cataract surgery. Usually this is mild and resolves with time and use of prescription eye drops. Rarely, however, severe inflammation can be encountered within a day or so of cataract surgery. One of the complications feared by experienced surgeons is Toxic Anterior Segement Syndrome (“TASS”) which is thought to be caused by a chemical or impurity that entered the eye during surgery. This is not an infection but requires early recognition and treatment (generally with prescription steroid drops) in order to prevent permanent loss of vision.
Infection
Following cataract surgery the most feared complication is endophthalmitis, an infection of the eye which can potentially lead to loss of vision. Left untreated, this complication can lead to blindness in hours or days. This is a true emergency. Fortunately, it is very rare, although certain eye conditions such as blepharitis are considered risk factors that can increase the likelihood of this complication. Symptoms of infection include significant or persistent pain in or around the eye, sudden or severe loss of vision, a very red eye, and significant discharge from the operated eye. Patients who suspect an infection should call their surgeon immediately, even if it’s 3 am! Immediate treatment of this complication is required if the vision is to be saved.
Retinal detachment
Retinal detachment may occur at any time (even years) after a perfectly successful cataract surgery. Although it can happen to anyone, there are certain risk factors for developing a retinal detachment. These include nearsigthedness (myopia), the occurrence of a posterior capsule tear during surgery, endophthalmitis, as well as other ocular conditions. Common symptoms of retinal detachment include sudden or severe loss of vision, flashes of light or multiple, new floaters or a shadow or curtain over the field of vision. If you notice any of these symptoms after your cataract surgery you should contact your doctor right away.
Periodic “flash” or “glints”
One of the side effects noted with the acrylic IOLs commonly used in the United States and Europe is that under certain lighting conditions they may reflect light such that eyes with these lenses may seem to periodically “flash”. Although a bit surprising at first, this does not affect vision and most people get used to this purely cosmetic side effect.
Lens Capsule Opacification
Once your cataract has been removed, it won’t come back. That being said, it is possible for your vision to become worse after surgery from what’s called posterior capsule opacification (PCO). Simply stated, the lens capsule shrink-wraps around the artificial lens implant (the eye heals a little too well) causing glare, halos, or blurred vision. The risk of this happening with a modern IOL is somewhere between 5% and 15%. This risk may be reduced if your eye doctor performs a procedure called “capsular polishing” during your cataract surgery. Fortunately, posterior capsular opacification can be removed with a laser treatment called YAG laser capsulotomy. The procedure creates a small hole/tear in the posterior capsule, is painless and takes only minutes to perform. There are very few risks of YAG laser capsulotomy, though those these do include transient elevation of the eye pressure and retinal detachment.
Dark or light crescents in the Peripheral Vision
Modern lenses are designed to limit the risk of posterior capsule opacification. However, this design occasionally results in the side effect of seeing a dark or light crescent to the side of one’s visual field. This condition, call “dysphotopsia” generally occurs under certain lighting conditions and tends to get better with time. Rarely, if symptoms are severe, treatment of this condition may require additional surgery to reposition or replace the IOL.
Lens Implant Power Issues
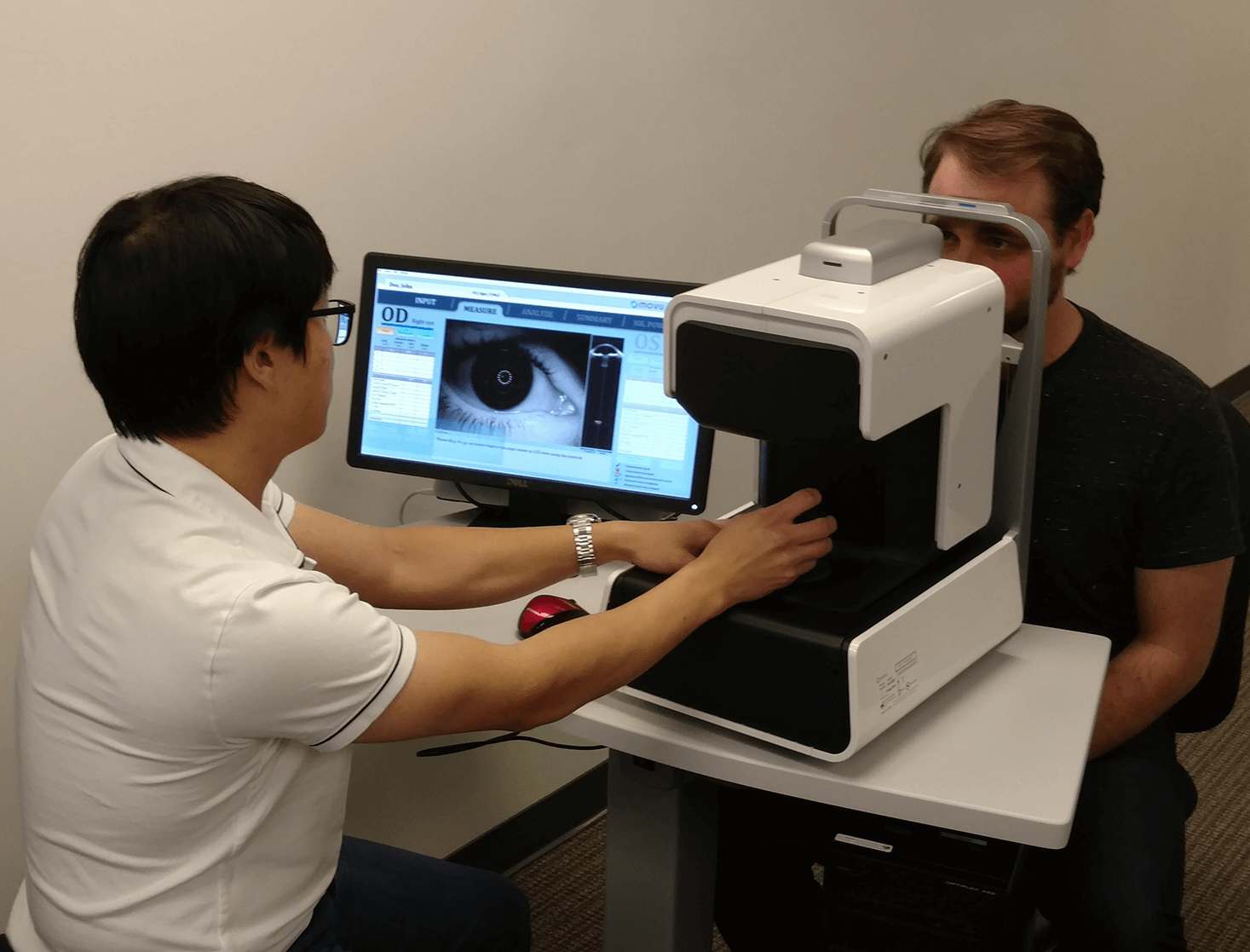
Measuring the Eye
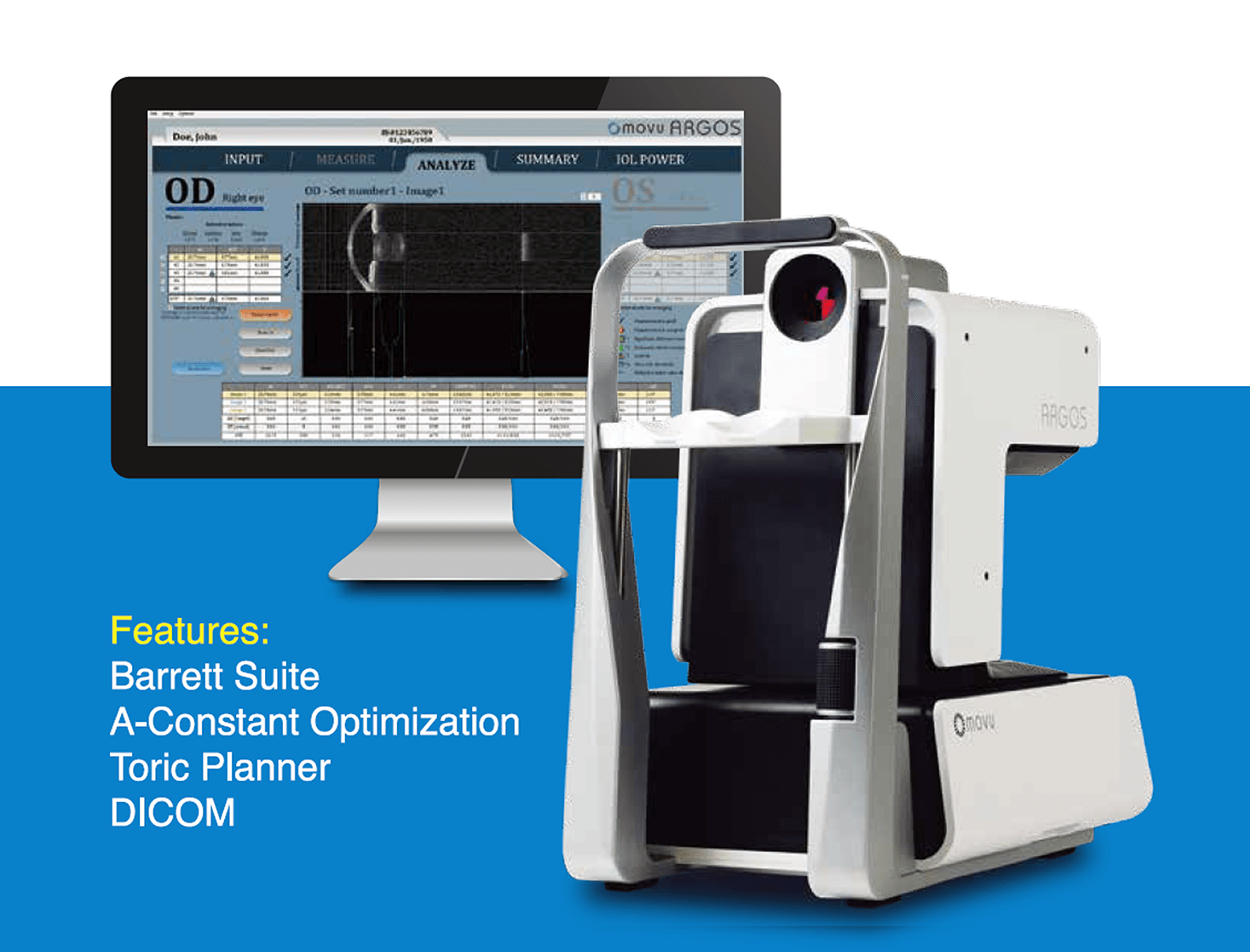
During cataract surgery the eye’s natural lens must be replaced with a synthetic lens implant. These implants must precisely focus light onto the retina in order to achieve clear vision. Similar to how contact lenses come in many different powers, intraocular lens implants also come in many different powers. Your eye surgeon must choose the lens power based on the structure of your eye. However, integral to the whole process is the accurate measurement of your eye prior to surgery. Using an Optical Biometer, your cataract surgeon measures essential parameters to determine the appropriate intraocular lens implant power and type. The more accurate the measurements, the better the visual outcome.
Eye Conditions May Impact the Quality of Eye Measurements
No matter how good the technology, the quality of the measurements will be impacted by various eye conditions. Risk factors for inaccurate measurements include the presence of dry eye. If present this may need to be treated with either over-the-counter or prescription eye drops or simple procedures such as eyelid cleansing prior to cataract surgery.
Unreasonable Expectations Can Lead to Disappointment
 The formulas and calculations your doctor uses to choose the artificial lens are imperfect in their ability to predict the correct lens implant power. Even with accurate measurements, modern diagnostic equipment, and high-quality intraocular lenses, it should be anticipated that vision could be further improved with prescription glasses or contact lenses even after cataract surgery. It is important to note that the standard monofocal lens implant is intended to replace the cataract but not the need for spectacles. In other words, the need to use prescription glasses after standard cataract surgery is not a complication—it should be expected. If you desire to reduce your dependence on prescription glasses after cataract surgery you should discuss the various intraocular lens options with your eye doctor prior to cataract surgery.
The formulas and calculations your doctor uses to choose the artificial lens are imperfect in their ability to predict the correct lens implant power. Even with accurate measurements, modern diagnostic equipment, and high-quality intraocular lenses, it should be anticipated that vision could be further improved with prescription glasses or contact lenses even after cataract surgery. It is important to note that the standard monofocal lens implant is intended to replace the cataract but not the need for spectacles. In other words, the need to use prescription glasses after standard cataract surgery is not a complication—it should be expected. If you desire to reduce your dependence on prescription glasses after cataract surgery you should discuss the various intraocular lens options with your eye doctor prior to cataract surgery.
Treatment of “Refractive Surprise”
If the intraocular lens power is significantly different than what was intended or desired and prescription spectacles or contact lens correction is not an acceptable treatment, then a refractive laser procedure or additional surgery such as a lens exchange may be considered. If a lens exchange procedure is being considered it is important to defer YAG laser capsulotomy until after lens exchange surgery as it is exceedingly difficult to remove and replace and IOL once the capsular bag has been broken. Potential complications of exchanging an IOL are similar to those of cataract surgery.
Intraocular Lens Dislocation
A torn posterior capsule or even certain eye disorders (such as prior eye trauma or pseudoexfoliation syndrome) can increase the risk that the artificial lens could move out of position resulting in blurred vision or glare. Sometimes a dislocated intraocular lens can be treated with new prescription eyeglasses. However, a severely dislocated intraocular lens often requires surgical repositioning or replacement.
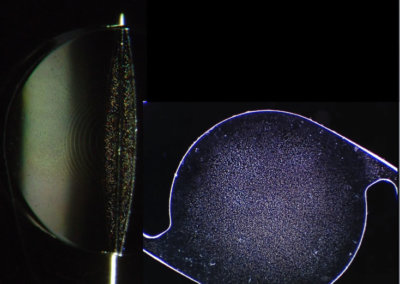
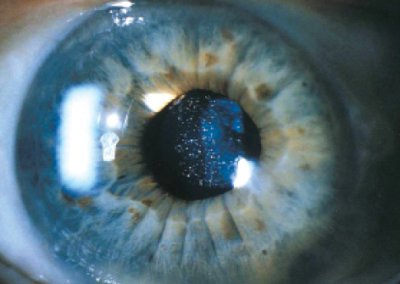
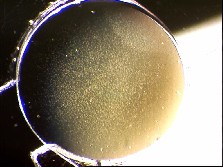
Hazy Vision Due To IOL Glistenings
 Cataracts result in blurred vision. The intraocular lenses inserted into the eye during cataract surgery are designed to produce clear vision. However, they are not without potential side effects. One such potential side effect is the development of “glistenings” (or nano-glistenings) which are microscopic fluid-filled bubbles that can form in synthetic lens material. A small number of glistenings may be observed in any lens implant that has been in the eye over a period of time. Patients generally don’t notice the effect of these small number of glistenings. However, large amounts of these glistenings may cause “hazy” vision along with increased glare at night.
Cataracts result in blurred vision. The intraocular lenses inserted into the eye during cataract surgery are designed to produce clear vision. However, they are not without potential side effects. One such potential side effect is the development of “glistenings” (or nano-glistenings) which are microscopic fluid-filled bubbles that can form in synthetic lens material. A small number of glistenings may be observed in any lens implant that has been in the eye over a period of time. Patients generally don’t notice the effect of these small number of glistenings. However, large amounts of these glistenings may cause “hazy” vision along with increased glare at night.
Hazy Vision Due to other Eye Disease
Sometimes there are no post cataract surgery problems, but the vision is still not clear. When this is the case, other conditions such as dry eyes, glaucoma, macular degeneration, or other eye diseases must be ruled out. Even mild eye disease can be significant with certain intraocular lenses (such as multifocal lenses).
Eyelid Droop
Not all cataract surgery complications involve the eyeball. Occasionally patients may note that the upper eyelid droops after a cataract procedure (this is called “ptosis”). If mild this can now be treated with prescription eye drops. If the droop is too severe to treat with eye drops then additional surgery on the eyelid may be required to “lift” the lid into a more natural position.
Summary of Cataract Operation Risks
Although there are many potential complications of cataract surgery, the overall risk of vision loss is quite low. You should now have a better idea of the various factors that must be considered by cataract patients prior to and following cataract surgery. Knowing about the various cataract surgery complications and their associated risks empowers you to increase your cataract surgery safety.
Why You Need to Know What IOL Your Eye Surgeon Will Implant During Cataract Surgery
Hazy Vision Due To Glistenings
Cataracts result in blurred vision. The intraocular lenses inserted into the eye during cataract surgery are designed to produce clear vision. However, they are not without potential side effects. One such potential side effect is the development of “glistenings” (or nano-glistenings) which are microscopic fluid-filled bubbles that can form in synthetic lens material. A small number of glistenings may be observed in any lens implant that has been in the eye over a period of time. Patients generally don’t notice the effect of these small number of glistenings. However, large amounts of these glistenings may cause “hazy” vision along with increased glare at night.
The Most Advanced Optical Biometer Is Now at San Marino Eye
The clarity of vision after cataract surgery greatly depends on the quality of measurements made by the surgeon prior to surgery. Dr. Richardson has invested in the most advanced optical biometer available: The ARGOS SS-OCT. With this advanced technology both
Dr. Richardson and his patients with cataracts can feel secure that they are getting the best eye measurements possible prior to choosing an intraocular lens.