Ab Interno
Canaloplasty
ABiC™—It’s Canaloplasty with an Elegant Twist!
Same Technology, Different Technique
What is Canaloplasty?
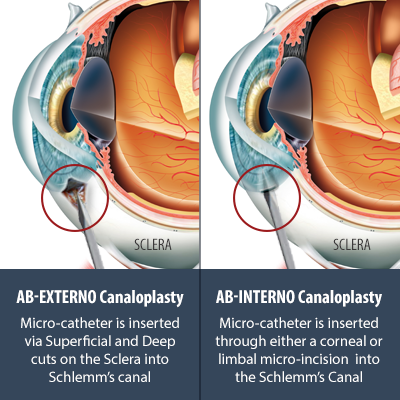
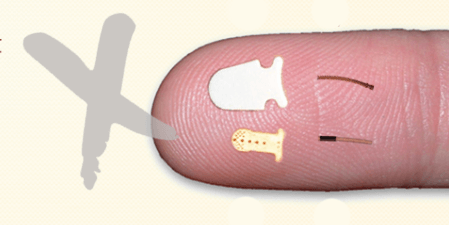
Canaloplasty is a non-penetrating (wall of the eye is not cut all the way through) glaucoma surgery developed by Dr. Robert Stegmann in 2008 with origins dating as far back 1968. It is an advanced surgical treatment for glaucoma which uses the world’s smallest micro-catheter to enlarge the eye’s natural drainage system. It is a safer but similarly effective surgery compared to penetrating surgeries (i.e. Trabeculectomy). More information about Ab-Externo Canaloplasty here.
What is Ab Interno Canaloplasty?
Recently, Dr. Mark Gallardo, developed a less invasive and much faster technique which is possibly as effective as Ab-Externo Canaloplasty: Ab-Interno Canaloplasty (ABiC™). The minimally invasive glaucoma surgery (MIGS) technique is not as tedious and complicated as the traditional canaloplasty and can be done by any skilled cataract surgeon.
Ab-Interno Canaloplasty: Same Technology, Different Technique
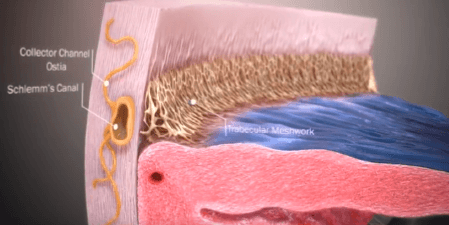
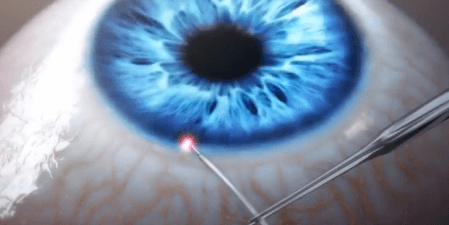
Canaloplasty uses an iTrack™ microcatheter to open the eye’s natural drainage system (“Schlemm’s canal”). Whereas, with traditional Canaloplasty, the Microcatheter is inserted from an external approach: cutting through the conjuctiva and sclera, with Ab-Interno Canaloplasty, the Micro-catheter is inserted from an internal approach: through either a clear corneal or a limbal micro-incision, then through a small opening in the Trabecular Meshwork, and into the Schlemm’s canal. With Ab-Interno, the eye tissue is preserved and not cut – no more flaps!
How Is ABiC™ Glaucoma Surgery Performed?
ABiC™ works by restoring the natural outflow pathways for aqueous humor, using a technique similar to angioplasty. During the procedure, ABiC™ comprehensively opens up all components of the eye’s natural outflow system – 1) Trabecular meshwork, 2) Schlemm’s canal, and 3) The Collector Channels and distal outflow system. Watch the video below to see the Simple Three-Step Procedure of ABiC™.
- First, your eye surgeon will make a small incision in the eye.
- The iTrack™ microcatheter is then inserted into the eye’s circumferential drainage canal. Your eye surgeon will advance the microcatheter 360 degrees around the canal to open up the channel and enlarge it.
- Once the end of the catheter has circumnavigated to its point of entry, the microcatheter tip is slowly pulled back while sterile, viscoelastic gel is injected into the canal to dilate it to 2-3 times its normal size. Enlarging and flushing through the drainage canal and adjacent outflow channels helps the aqueous fluid to drain properly. The microcatheter is then withdrawn from the eye.
- No permanent implants or devices left in the eye.
- Restores the eyes natural drainage system
- improve fluid outflow
- reduce the pressure inside your eye
- Can also reduce or even eliminate glaucoma medications.
Ab-Interno Canaloplasty: Benefits Over Other MIGS Options
Restoration of the Eye’s Natural Drainage Channels
- 360 degrees of Schlemm’s canal (as opposed to on a small fraction of the canal)
- Collector channel system (no other MIGS addresses this portion of the drainage system)

Future Surgery Is Not Compromised
As such, it’s generally a better course of action to perform ABiC™ first
ABiC™ is Non-destructive
The trabecular meshwork (TM) which has an active role in regulation of drainage, remains intact after ABiC™. In contrast, the trabecular meshwork is destroyed with Trabectome and Kahook Dual Blade trabeculotomy.
No Permanent Implant or Stent
Better Clinical Outcomes
Covered by Medicare
As of June 2018 this is not the case with the iStent or CyPass.
Ab Interno Canaloplasty (ABiC™) Safety and Efficacy
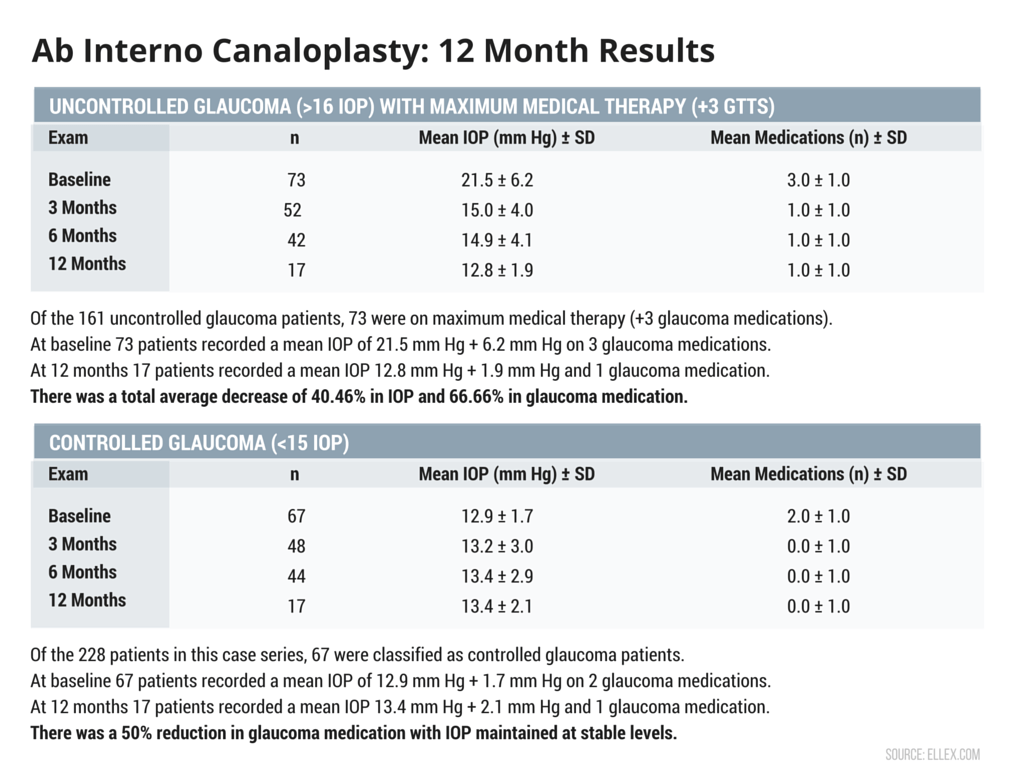
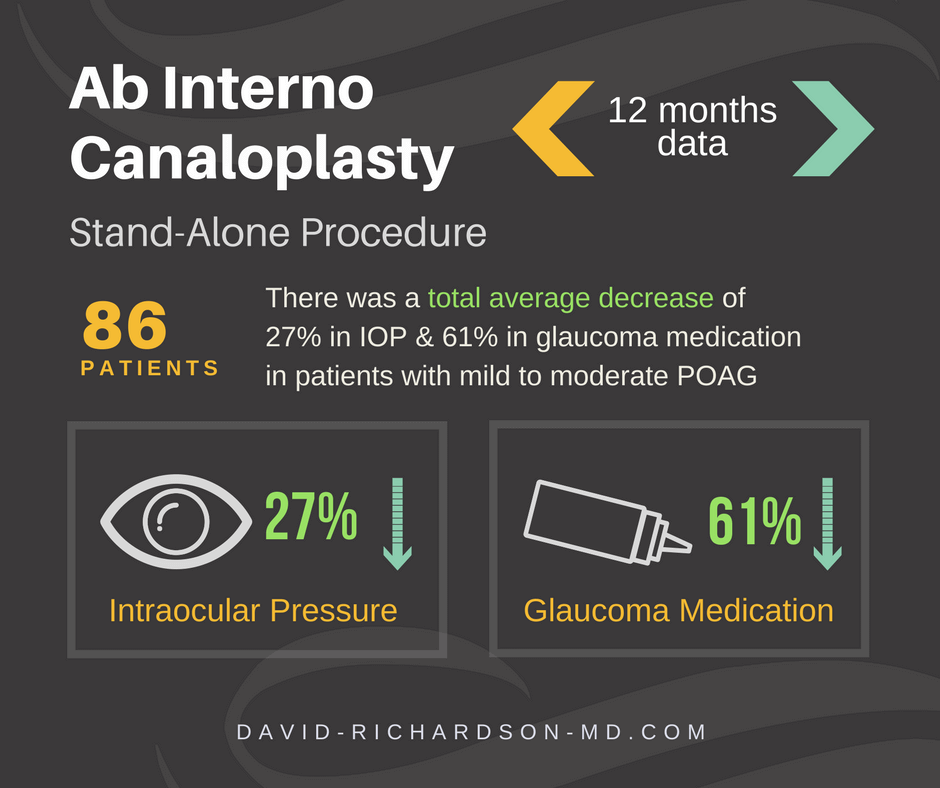
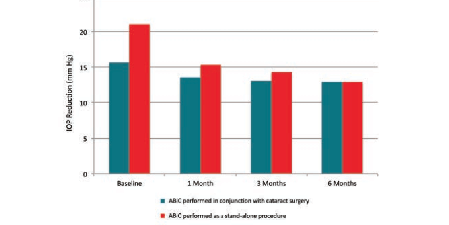
Is ABiC™ Safe and Effective? Yes, Ab Interno Canaloplasty has an incredible safety profile. Unlike other currently available MIGS procedures, ABiC™ preserves tissue and does not require permanent placement of an implant in the eye. Not only is ABiC™ safer compared to traditional glaucoma surgeries, it is also effective. On average, it achieves a reduction in mean IOP of 30%, combined with a 50% reduction in medication dependence.
Interim 24-Month Data – Mark J. Gallardo, MD (USA)
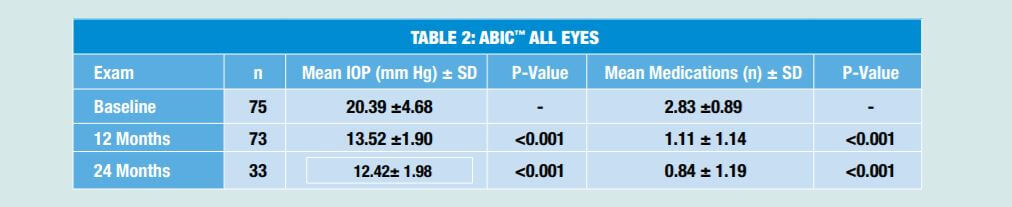
Seventy five patients (75 eyes) with mild to moderate primary open angle glaucoma (POAG) were enrolled in the study. At 24 months postoperatively there was a 39.06% reduction in mean IOP, as compared to baseline, and a 70.15% reduction in the mean number of medications.
Source: Ellex.com | Download Whitepapter | (Interim data only. Not published.)
Interim 18-Month Data – Mahmoud A. Khaimi, MD (USA)
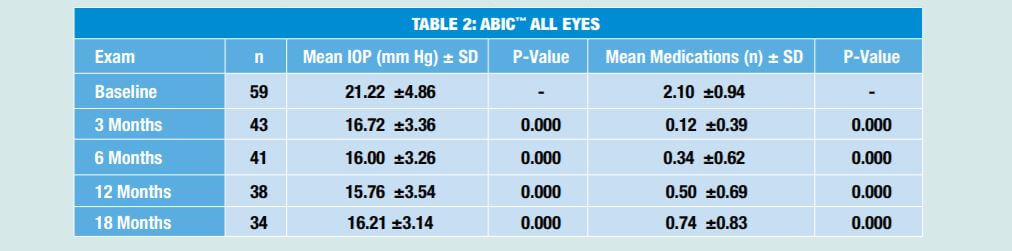
Fifty nine patients (59 eyes) with mild to moderate primary open angle glaucoma (POAG) were enrolled in the study. At 18 months postoperatively there was a 23.6% reduction in mean IOP, as compared to baseline, combined with a 64.8% reduction in the mean number of medications.
Source: Ellex.com | Download Whitepaper | (Interim data only. Not published.)
12-Month Data – Professor Norbert Koerber FEBO (Germany)
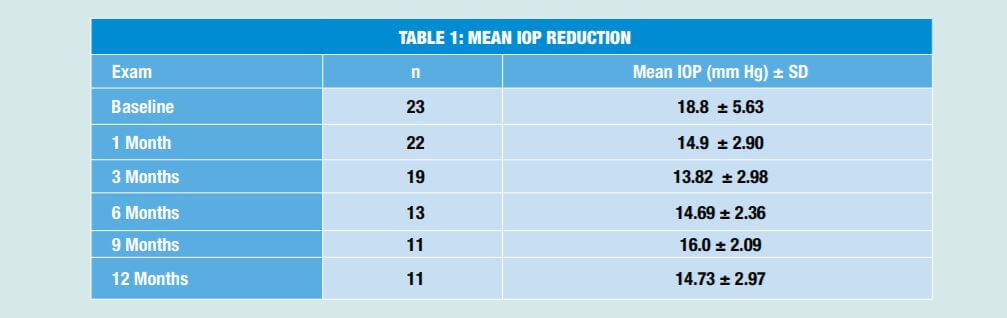
Twenty-three patients (23 eyes) were enrolled in the study. Mean IOP reduced from 18.8 ± 5.63 mm Hg preoperatively to 14.73 ± 2.97 (n=11) at 12 months postoperatively. The mean number of medications was reduced from 1.69 preoperatively to 0.21 at the last follow-up visit.
There was one reported complication of limited descemetolysis near the limbus by the viscoelastic during the dilatation of Schlemm`s canal. No adverse events as a result of the device were reported.
Source: Ellex.com | Download Whitepaper
What are the side effects of ABiC?
Ab Interno Canaloplasty is associated with significantly fewer risks, both in number and severity, than traditional glaucoma surgeries. However, all surgeries have risks associated with them. The most common risks associated with ABiC™ are:
- Bleeding in the Eye
- Intraocular Pressure “Spikes”
- The Formation of a Bleb
- Hypotony (IOP too low)
What if ABiC doesn’t work for me?
A key benefit of ABiC™ is that is does not limit future (other form of) glaucoma treatment. If the procedure is not successful, your surgeon may perform laser-based treatment, such as SLT, Ab-Externo Canaloplasty or traditional glaucoma surgery (trabeculectomy). Medication may also be an option.
Does ABiC hurt?
Who Is a Candidate For Ab-Interno Canaloplasty Surgery?
Most anyone with open angle glaucoma that requires treatment is a candidate for Canaloplasty.
ABiC™ is also suitable for the following:
- Open Angle Glaucoma with ocular surface disease
- Pigmentary Glaucoma (PG)
- Pseudoexfoliation Glaucoma (PXF)
- Ocular Hypertension
- Normal Tension Glaucoma (NTG)
- Juvenile Glaucoma
- Steroid Induced Glaucoma
- Patients Post-SLT
- Patients who can’t keep up with Drops Regimen – a hassle and/or too costly
- Patients Post single session low power ALT
- Patients with previous failed trabeculectomy or tube surgery in which Schlemm’s canal has been left undamaged from previous filtrating surgeries.
- Open Angle Glaucoma with narrow but not occludable angles after laser iridotomy
Who Is NOT a Candidate For ABiC™ Surgery?
Ab-Interno Canaloplasty is contraindicated for the following:
- Open Angle Glaucoma with ocular surface disease
- Pigmentary Glaucoma (PG)
- Pseudoexfoliation Glaucoma (PXF)
- Ocular Hypertension
- Normal Tension Glaucoma (NTG)
- Juvenile Glaucoma
- Steroid Induced Glaucoma
- Patients Post-SLT
Canaloplasty Has Helped Many Glaucoma Patients
These are just a few testimonials out of over 60,000 canaloplasty procedures done worldwide!
So I said, “Well we know about me, I don’t like drops, I don’t do them well, laser didn’t work. Can we go right to canaloplasty on the left eye?” And that’s exactly what we did. All in all it was absolutely the right decision, for me. Given who I was, my lifestyle, the way I work, and what I wanted. So it’s an excellent result…It was absolutely the right decision.
My first expression when it was over was that “It was a piece of cake!” And I would recommend it to people because I think it was very successful and the biggest part about it, aside from not losing anymore eyesight, I don’t have to take drops four and five times a day. Four and five drops, four and five times a day. So I was very happy with that outcome also.
There are a lot of costs involved when it comes to travelling all the way from India and then coming here. But seeing the plus points in terms of …physical activities… And seeing that I don’t have to undergo lifestyle modification it’s (cost) hardly anything. And I don’t regret the decision of coming here and getting the surgery done – at all.I’m truly very happy.
So I checked around and canaloplasty came up… (Duke Eye Center)—mentioned canaloplasty. And I called up another friend of mine who is a chair of UC Irvine and he recommended the same thing….
April 20, 2012 | Chicago, IL – Dr. Robert Sinkey was interviewed by Dr. David Richardson at an iScience didactic course during the American Society of Cataract and Refractive Surgery (ASCRS) 2012 annual meeting. Dr. Sinskey discussed his glaucoma diagnosis, treatment and decision to have Canaloplasty as well as the subsequent outcomes of the procedure.
What Top Glaucoma Surgeons Are Saying
Because ABiC™ is minimally invasive and relatively atraumatic, it can be used in a broad spectrum of patients. It can be a first-line, standalone procedure for the treatment of uncontrolled glaucoma that requires surgical intervention in both phakic and pseudophakic patients. In those whose glaucoma is well-controlled via topical therapy, ABiC™ can be used adjunctively in cataract surgery to reduce the medication burden. In eyes with uncontrolled glaucoma, ABiC™ may reduce IOP and avoid filtration surgery during cataract surgery.
I also like to use ABiC™ in monocular patients, because it has such a great risk-benefit profile, can be performed under topical anaesthesia, and it provides almost immediate recovery along with an excellent reduction in IOP.
ABiC has also proven to be highly effective in cases of controlled glaucoma. In a recent case series of 122 eyes followed
over 12 months, my colleagues and I used ABiC™ to effectively reduce the medication burden of controlled glaucoma patients (<15 mm Hg IOP) by an average of 50%, while maintaining mean IOP at 12.8 mm Hg.
The postoperative regimen for ABiC™ is similar to that for cataract surgery. I prescribe topical antibiotics and a low-dose topical steroid for 3 to 4 weeks, and instruct patients not to engage in extreme lifting or bending. That is it. With trabeculectomy and glaucoma drainage implants, patients are usually prescribed drops for at least 2 months, and no physical exertion for up to 8 weeks. From a quality-of-life perspective, those are big differences.
ABiC™ is safe and effective in achieving IOP reduction and reduces dependence on anti-glaucoma medications in patients with OAG, both as a standalone procedure and combined with phacoemulsification.
Ab-Interno Canaloplasty is a microinvasive glaucoma surgery (MIGS) procedure that’s just been developed as an enhancement of Canaloplasty. The technique is not as tedious and complicated as the traditional canaloplasty and can be done by any skilled cataract surgeon.
Canaloplasty has been available for a number years. We have long-term results with the Ab-Externo (traditional) Canaloplasty and they look really good! Additional studies will still be necessary to confirm that ABiC™ works as well and as long as Ab-Externo Canaloplasty. However, given its incredible safety profile combined with moderate IOP reduction, ABiC is poised to be an ideal surgical treatment option for anyone with uncontrolled moderate open angle glaucoma. By far, in my opinion, ABiC™, is the most promising, of the microinvasive glaucoma surgeries.
The ideal patient, I would say, shows progression in the optical coherence tomography but does not yet show a visual field defect. The second indication is intolerance to drugs, whatever IOP the patient has. I would even perform ABiC in a patient who has a pressure of 14 mm Hg but is taking three medications and has bad tolerance. The
patients are so happy later. I get many letters from patients telling me how happy they are because their quality of life has improved. They just feel better. The burden and the side effects of the medications are gone, and they can finally relax. I think we often do not realize how much we improve lives by taking patients off medications.
What I love so much about ABiC™ is that it works on multiple pathways. One of the issues we face with any MIGS device is the fact that preoperatively, we do not always understand where the resistance to outflow is occurring. Each one of the devices on the market works
to enhance a different part of the natural outflow system. The advantage of ABiC™ is that instead of working on just one part of the pathway, it works on dilating Schlemm canal and improving function of the trabecular meshwork and distal collector channels. I think this kind of comprehensive approach to the natural outflow systems is the primary benefit of ABiC™.
LATEST ARTICLES ON DR. RICHARDSON’S GLAUCOMA HEALTHHUB
See If Canaloplasty Is for You
David D. Richardson, MD, is a board-certified Ophthalmologist specializing in the treatment of cataract and glaucoma. He is also recognized as one of the most highly skilled cataract and glaucoma surgeons in the US and is among an elite group of glaucoma surgeons in the country performing the highly specialized, minimally-invasive glaucoma surgery (MIGS), canaloplasty.
Call today to schedule an appointment with Dr. Richardson at
(626) 289 7856